Anti-inflammatory Biomolecule for the Suppression of LPS-induced Cytokine Storms
Natural fatty acid binding proteins suppress LPS-activated inflammatory responses mediated by TLR4, suggested to have a role in COVID-19
Background
During bacterial infections, high levels of lipopolysaccharides (LPS) in blood plasma may trigger an uncontrolled systemic inflammatory response known as sepsis. This inflammatory response to microbial endotoxins may progress to septic shock, in which the blood supply to internal organs dramatically decreases. Septic shock is a life-threatening condition that can dangerously lead to multiple organ failure and subsequent death. According to the Centers for Disease Control and Prevention, at least 1.7 million adult Americans develop sepsis each year, of which nearly 270,000 die.
Toll-like receptor 4 (TLR4) is an innate immune receptor that recognizes bacterial LPS. This transmembrane protein plays a critical role in the signaling pathways that induce cytokine storms and elicit inflammatory responses. Therefore, the scientific community is actively looking for antagonists that block the activation of TLR4 to prevent the downstream signaling cascades that trigger inflammatory responses during sepsis and septic shock.
Technology Overview
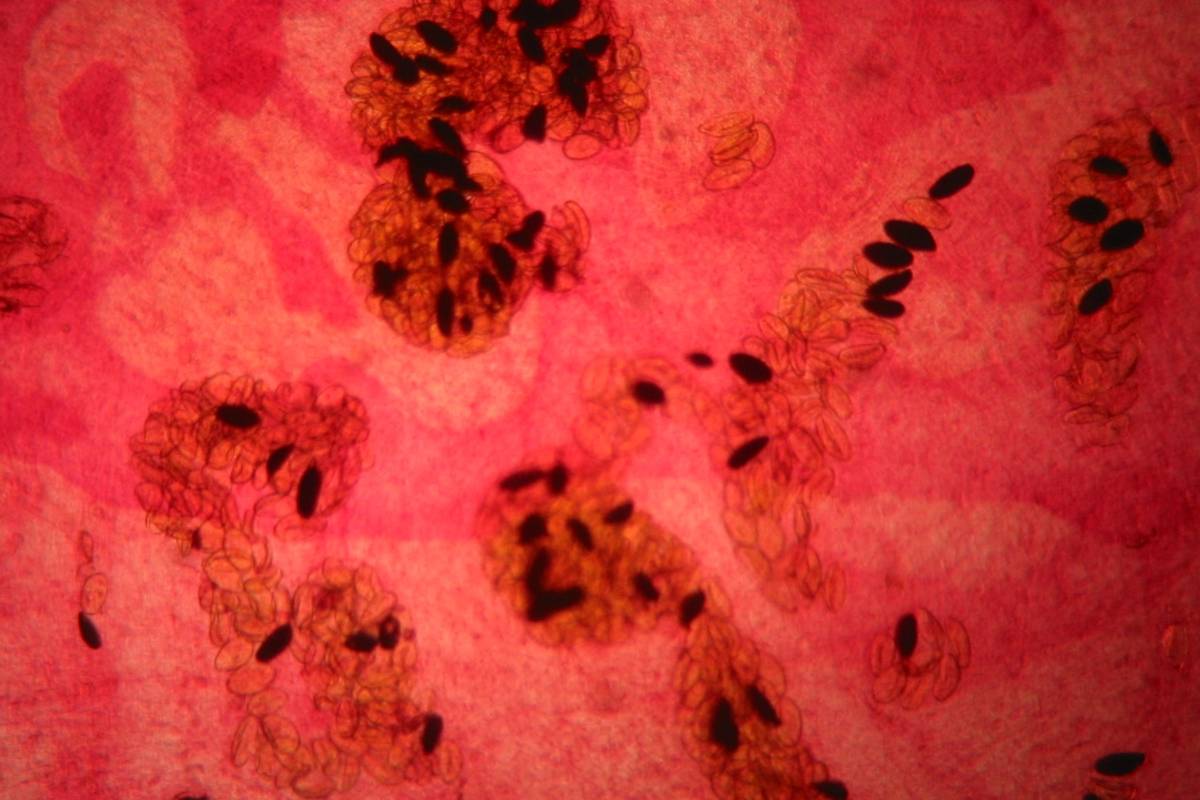
Fasciola hepatica, the parasitic helminth that causes fascioliasis in humans and other mammals, has the powerful capacity to evade or modify the immune responses of its hosts for long periods of time. Polypeptide components of F. hepatica excretory-secretory products (ESP) are responsible for the powerful suppression of the host’s immune responses. Fatty Acid Binding Proteins (FABP) present in the ESPs have been found to provide protection against oxidative damage to cellular components of the helminth by binding fatty acids and ions involved in oxidative stress.
A purified form of F. hepatica’s FABP, denominated Fh12, has demonstrated a potent anti-inflammatory capacity, suppressing the LPS-induced expression of inflammatory cytokines both in vitro and in vivo. Fh12 binds to CD14, a co-receptor of TLR4, blocking interactions between TLR4 and LPS, thus preventing the activation of inflammatory cytokines. In mouse bone marrow derived macrophages (bmMΦs), Fh12 alone does not induce cytokine expression. In contrast, Fh12 suppressed IL12, TNFα, IL6 and IL1β cytokines as well as the phosphorylation of ERK, p38 and JNK mitogen-activated protein kinases in bmMΦs in response to LPS. Furthermore, Fh12 impaired bmMΦs phagocytic capacity and suppressed iNOS2, an LPS-inducible enzyme. Fh12 blocks the entire TLR4 pathway on HEK293-TLR4 cells, as suggested by the suppression of NF-κB transcription factor in a dose dependent manner, but independent of LPS exposure duration.
A single intraperitoneal injection of 15μg of the purified Fh12 protein to the C57BL/6 mouse model of septic shock 1-hour prior exposure to LPS significantly suppressed the expression of serum pro-inflammatory and inflammatory cytokines IFNγ, IL12p70, TNFα, GM-CSF, IL3, IL9, IL10, and IL15 after exposure, demonstrating as well immunoprophylactic properties against inflammation induction by LPS.
Due to the growing emergence of bacterial multi-antibiotic resistance, nosocomial infections are becoming harder to treat. Fh12 could become an important biomolecule for the development of therapeutic alternatives to treat sepsis and septic shock, or even as a prophylactic option to prevent the activation of inflammatory cytokines storms during bacterial infections. Fh12 may further represent a promising alternative to prevent the symptoms of other inflammatory diseases like ischemia/reperfusion injury, and several neurodegenerative and neurological disorders associated with an increased expression of TLR4 in microglial cells.
Further Details:
- Martin I, Cabán-Hernández K, Figueroa-Santiago O, Espino AM (2015) Fasciola hepatica Fatty Acid Binding Protein Inhibits TLR4 Activation and Suppresses the Inflammatory Cytokines Induced by Lipopolysaccharide In Vitro and In Vivo. J Immunol 194:3924–3936. https://doi.org/10.4049/jimmunol.1401182. PMC4390499
Benefits
- Sepsis inflammatory response suppression and prevention
- Potential for combination or alternative therapies
- Possible treatment for TLR4 associated pathologies
- Drug development to block inflammatory responses
Applications
- Potentially prevent and treat diseases known to be mediated by TLR4:
- Sepsis / Septic shock
- Ischemia/reperfusion injury
- Neuroinflammatory disorders associated to TLR4 overexpression
- Alzheimer’s disease
- Parkinson’s disease
- Amyotrophic Lateral Sclerosis
- Inflammatory Bowel Disease (IBD)
- Other diseases mediated by TLR4
- TLR4 has been suggested to have a role in COVID-19-associated inflammation
- Choudhury, A.; Mukherjee, S. In Silico Studies on the Comparative Characterization of the Interactions of SARS-CoV-2 Spike Glycoprotein with ACE-2 Receptor Homologs and Human TLRs. J. Med. Virol. 2020. https://doi.org/10.1002/jmv.25987.
- Andersson, U.; Ottestad, W.; Tracey, K. J. Extracellular HMGB1: A Therapeutic Target in Severe Pulmonary Inflammation Including COVID-19? Mol. Med. 2020, _26_ (1), 42. https://doi.org/10.1186/s10020-020-00172-4.
Opportunity
- Exclusive or non-exclusive license
- Research support for additional development